
Book an appointment
Diagnostic and Therapeutic Endoscopy
A therapeutic endoscopic procedure provides treatment that is carried out via the endoscope. A procedure, which starts as a diagnostic or screening endoscopy, may become a therapeutic endoscopy depending on what is visualized during the procedure.
ERCP

Endoscopic retrograde cholangiopancreatography
Endoscopic retrograde cholangiopancreatography, or ERCP, is a procedure to diagnose and treat problems in the liver, gallbladder, bile ducts, and pancreas. It combines X-ray and the use of an endoscope—a long, flexible, lighted tube. Your healthcare provider guides the scope through your mouth and throat, then down the esophagus, stomach, and the first part of the small intestine (duodenum). Your healthcare provider can view the inside of these organs and check for problems. Next, he or she will pass a tube through the scope and inject a dye. This highlights the organs on X-ray.
Why might I need ERCP?
You may need ERCP to find the cause of unexplained abdominal pain or yellowing of the skin and eyes (jaundice). It may be used to get more information if you have pancreatitis or cancer of the liver, pancreas, or bile ducts.
Other things that may be found with ERCP include:
- Blockages or stones in the bile ducts
- Fluid leakage from the bile or pancreatic ducts
- Blockages or narrowing of the pancreatic ducts
- Tumors
- Infection in the bile ducts
Your healthcare provider may have other reasons to recommend an ERCP.
What are the risks of ERCP?
You may want to ask your healthcare provider about the amount of radiation used during the test. Also ask about the risks as they apply to you.
Consider writing down all X-rays you get, including past scans and X-rays for other health reasons. Show this list to your provider. The risks of radiation exposure may be tied to the number of X-rays you have over time.
If you are pregnant or think you could be, tell your healthcare provider. Radiation exposure during pregnancy may lead to birth defects.
Tell your healthcare provider if you are allergic to or sensitive to medicines, contrast dyes, iodine, or latex.
Some possible complications may include:
- Inflammation of the pancreas (pancreatitis) or gallbladder (cholecystitis). Pancreatitis is one of the most common complications and should be discussed with your provider ahead of time. Keep in mind, though, that ERCP is often performed to help relieve the disease in certain types of pancreatitis.
- Infection
- Bleeding
- A tear in the lining of the upper section of the small intestine, esophagus, or stomach
- Collection of bile outside the biliary system (biloma)
You may not be able to have ERCP if:
- You’ve had gastrointestinal (GI) surgery that has blocked the ducts of the biliary tree
- You have pouches in your esophagus (esophageal diverticula) or other abnormal anatomy that makes the test difficult to perform. Sometimes the ERCP is modified to make it work in these situations.
- You have barium within the intestines from a recent barium procedure since it may interfere with an ERCP
There may be other risks depend based on your condition. Be sure to discuss any concerns with your healthcare provider before the procedure.
How do I get ready for ERCP?
Recommendations for ERCP preparation include the following:
- Your healthcare provider will explain the procedure and you can ask questions.
- You may be asked to sign a consent form that gives your permission to do the test. Read the form carefully and ask questions if something is not clear.
- Tell your healthcare provider if you have ever had a reaction to any contrast dye, or if you are allergic to iodine.
- Tell your healthcare provider if you are sensitive to or are allergic to any medicines, latex, tape, or anesthesia.
- Do not to eat or drink liquids for 8 hours before the procedure. You may be given other instructions about a special diet for 1 to 2 days before the procedure.
- If you are pregnant or think you could be, tell your healthcare provider.
- Tell your healthcare provider of all medicines (prescribed and over-the-counter) and herbal supplements that you are taking.
- Tell your healthcare provider if you have a history of bleeding disorders or if you are taking any blood-thinning medicines (anticoagulants), aspirin, ibuprofen, naproxen, or other medicines that affect blood clotting. You may be told to stop these medicines before the procedure.
- If you have heart valve disease, your healthcare provider may give you antibiotics before the procedure.
- You will be awake during the procedure, but a sedative will be given before the procedure. Depending on the anesthesia used, you may be completely asleep and not feel anything. You will need someone to drive you home.
- Follow any other instructions your provider gives you to get ready.
What happens during ERCP?
An ERCP may be done on an outpatient basis or as part of your stay in a hospital. Procedures may vary based on your condition and your healthcare provider’s practices.
Generally, an ERCP follows this process:
- You will need to remove any clothing, jewelry, or other objects that may interfere with the procedure.
- You will need to remove clothes and put on a hospital gown.
- An intravenous (IV) line will be put in your arm or hand.
- You may get oxygen through a tube in your nose during the procedure.
- You will be positioned on your left side or, more often, on your belly, on the X-ray table.
- Numbing medicine may be sprayed into the back of your throat. This helps prevent gagging as the endoscope is passed down your throat. You will not be able to swallow the saliva that collects in your mouth during the procedure. It will be suctioned from your mouth as needed.
- A mouth guard will be put in your mouth to keep you from biting down on the endoscope and to protect your teeth.
- Once your throat is numbed and you are relaxed from the sedative. Your provider will guide the endoscope down the esophagus into the stomach and through the duodenum until it reaches the ducts of the biliary tree.
- A small tube will be passed through the endoscope to the biliary tree, and contrast dye will be injected into the ducts. Air may be injected before the contrast dye. This may cause you to feel fullness in your abdomen.
- Various X-ray views will be taken. You may be asked to change positions during this time.
- After X-rays of the biliary tree are taken, the small tube for dye injection will be repositioned to the pancreatic duct. Contrast dye will be injected into the pancreatic duct, and X-rays will be taken. Again, you may be asked to change positions while the X-rays are taken.
- If needed, your provider will take samples of fluid or tissue. He or she may do other procedures, such as the removal of gallstones or other blockages, while the endoscope is in place.
- After the X-rays and any other procedures are done, the endoscope will be withdrawn.
What happens after ERCP?
After the procedure, you will be taken to the recovery room. Once your blood pressure, pulse, and breathing are stable and you are alert, you will be taken to your hospital room or discharged home. If this procedure was done as an outpatient, plan to have someone drive you home.
You will not be allowed to eat or drink anything until your gag reflex has returned. You may have a sore throat and pain with swallowing for a few days. This is normal.
Many times, a rectal suppository of a certain medicine is given after the ERCP to decrease the risk of pancreatitis.
You may go back to your usual diet and activities after the procedure, unless your healthcare provider tells you otherwise.
Tell your healthcare provider if you have any of the following:
- Fever or chills
- Redness, swelling, or bleeding or other drainage from the IV site
- Abdominal pain, nausea, or vomiting
- Black, tarry, or bloody stools
- Trouble swallowing
- Throat or chest pain that worsens
Your healthcare provider may give you other instructions after the procedure, based on your situation.
Next steps
Before you agree to the test or the procedure make sure you know:
- The name of the test or procedure
- The reason you are having the test or procedure
- What results to expect and what they mean
- The risks and benefits of the test or procedure
- What the possible side effects or complications are
- When and where you are to have the test or procedure
- Who will do the test or procedure and what that person’s qualifications are
- What would happen if you did not have the test or procedure
- Any alternative tests or procedures to think about
- When and how will you get the results
- Who to call after the test or procedure if you have questions or problems
- How much will you have to pay for the test or procedure
EUS

Overview
Endoscopic ultrasound (EUS) is a minimally invasive procedure to assess digestive (gastrointestinal) and lung diseases. A special endoscope uses high-frequency sound waves to produce detailed images of the lining and walls of your digestive tract and chest, nearby organs such as the pancreas and liver, and lymph nodes.
EUS techniques are also used in certain treatments, such as draining pseudocysts.
Why it’s done
EUS is used to find the cause of symptoms such as abdominal or chest pain, to determine the extent of diseases in your digestive tract and lungs, and to evaluate findings from imaging tests such as a CT scan or MRI.
EUS may help in the evaluation of:
- Cancer of the colon, esophagus, lung, pancreas or stomach, and ampullary and rectal cancers
- Lymphoma
- Barrett’s esophagus
- Neuroendocrine tumors
- Pancreatitis and pancreatic cysts
- Bile duct stones
- Sarcoidosis
EUS can help:
- Assess how deeply a tumor penetrates your abdominal wall in esophageal, gastric, rectal, pancreatic and lung cancers
- Determine the extent (stage) of cancer, if present
- Determine if cancer has spread (metastasized) to your lymph nodes or other organs
- Provide precise information about non-small cell lung cancer cells, to guide treatment
- Evaluate abnormal findings from imaging tests, such as cysts of the pancreas
- Guide drainage of pseudocysts and other abnormal collections of fluid in the abdomen
- Permit precise targeting for delivering medication directly into the pancreas, liver and other organs
EUS is performed on an outpatient basis and is well-tolerated by most people.
You may not be a candidate for EUS if you have had abdominal surgery that changed your anatomy, such as Roux-en-Y gastric bypass.
Risks
EUS is generally safe when performed at a center with an experienced and expert health care team. Your doctor will discuss with you the risk of complications from EUS. These risks are most commonly associated with fine-needle aspiration.
Risks may include:
- Bleeding
- Infection
- Tearing (perforation) of the intestinal wall or throat
- Pancreatitis, if fine-needle aspiration of the pancreas is done
You can reduce your risk of complications by carefully following your doctor’s instructions for preparing for EUS.
Call your doctor immediately or go to an emergency room if you experience any of the following signs or symptoms:
- Fever
- Chest pain
- Shortness of breath
- Black or very dark-colored stool
- Severe or persistent abdominal pain
How you prepare
Your doctor will give you specific instructions to prepare for your EUS. You may be asked to:
- Fast before EUS. to make sure your stomach is empty. Generally, you’ll be asked to fast for at least 6 hours before the test.
- Prepare your rectum, if EUS is being done in the rectal area. You may be asked to take a laxative or have an enema and to follow a liquid diet before the procedure.
- Stop taking certain medications, such as blood thinners. Blood thinners may increase your risk of bleeding if fine-needle aspiration is performed during EUS. If you have chronic conditions, such as diabetes or high blood pressure, your doctor will give you specific instructions regarding your medications.
- Plan ahead for your recovery, if you will be sedated before EUS. Most people who have EUS are given medication to relax them. Arrange for someone to drive you home after the procedure.
What you can expect
You likely will be given medicine to help you relax.
During EUS your doctor passes a thin, flexible tube (endoscope) through your mouth and through your digestive tract. A small ultrasound device (transducer) in the tube produces sound waves that create a precise image of surrounding tissue, including lymph nodes in the chest. The endoscope is then gradually withdrawn.
If you have fine-needle aspiration with EUS, your doctor may need to pass a second, curved device through a channel in the endoscope into your digestive tract. That device can guide a very slender needle to your lymph nodes and tumors or other abnormalities. The needle extracts fluid and tissue for analysis.
EUS with fine-needle aspiration generally lasts less than an hour.
Results
A specialist in digestive diseases (gastroenterologist) or lung disease (pulmonologist) with special training in EUS will interpret the EUS images. A doctor trained in analyzing biopsies (pathologist) will report the test results if you have fine-needle aspiration. Your doctor will discuss any important findings and next steps with you.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
EMR
Overview
Gastrointestinal endoscopic mucosal resection (EMR) is a procedure to remove precancerous, early-stage cancer or other abnormal tissues (lesions) from the digestive tract.
Endoscopic mucosal resection is performed with a long, narrow tube equipped with a light, video camera and other instruments. During EMR of the upper digestive tract, the tube (endoscope) is passed down your throat to reach an abnormality in your esophagus, stomach or upper part of the small intestine (duodenum).
To remove lesions from the colon, the tube is guided up through the anus.
Primarily a treatment procedure, EMR is also used to collect tissues for diagnosis. If cancer is present, EMR can help determine if the cancer has invaded tissues beneath the digestive tract lining.
Why it’s done
Endoscopic mucosal resection is a less invasive alternative to surgery for removing abnormal tissues from the lining of the digestive tract. These tissues may be:
- Early-stage cancer
- Precancerous lesions, which may become cancerous
Endoscopic mucosal resection is usually performed by a specialist in digestive system disorders (gastroenterologist) who has expertise in this technique.
Risks
Risks of the endoscopic mucosal resection include:
- Bleeding. This most common complication often can be detected and corrected during the procedure.
- Narrowing of the esophagus. Removing a lesion that encircles the esophagus carries some risk of scarring that narrows the esophagus, a condition that may lead to difficulty swallowing and require further treatment.
- Puncture (perforation). There is a slight risk of a puncture through the wall of the digestive tract, depending on the size and location of the lesion that’s removed.
Call your doctor or get emergency care if you develop any of the following signs or symptoms after undergoing endoscopic mucosal resection:
- Fever
- Chills
- Vomiting
- Black stool
- Bright red blood in the stool
- Chest or abdominal pain
- Shortness of breath
- Fainting
How you prepare
Before you have endoscopic mucosal resection, you’ll be asked to provide the following information:
- All prescription medications, over-the-counter drugs and dietary supplements you take — particularly diabetes medications and blood-thinning drugs, including aspirin — and their doses
- Drug allergies
- All medical conditions, including heart disease, lung disease, diabetes and blood-clotting disorders
Your doctor may ask you to temporarily stop taking some medications, including those that affect blood clotting or those that interfere with sedatives before the procedure.
You’ll receive written instructions about what to do the day before the procedure. These instructions may vary depending on the location of the lesion or lesions being removed. In general, the instructions will likely include:
- Fasting. You’ll be instructed when to begin fasting. You may not be able to eat, drink, chew gum or smoke after midnight before the procedure. You may be asked to be on a clear liquid diet the day before your procedure.
- Cleaning the colon. If the procedure involves the colon, you’ll likely use a liquid laxative or an over-the-counter enema kit to empty your bowels and clean your colon.
You’ll also sign an informed consent document giving your doctor permission to perform the procedure after the risks and benefits have been explained to you. Before you sign the form, ask your doctor about anything you don’t understand about the procedure.
Travel arrangements
You’ll likely go home the day of your EMR. However, because of sedation used during the procedure, you’ll need to have someone take you home.
What you can expect
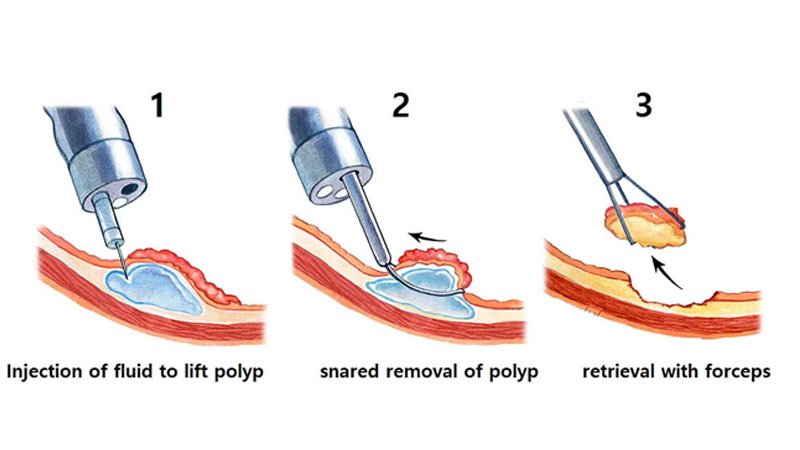
There are a few versions of endoscopic mucosal resection. Ask your gastroenterologist about how your procedure will be performed. A common approach includes these steps:
- Inserting the endoscope and guiding the tip to the area of concern
- Injecting a fluid under a lesion to create a cushion between the lesion and healthy tissue underneath it
- Lifting the lesion, possibly using gentle suction
- Cutting the lesion to separate it from surrounding healthy tissue
- Removing the abnormal tissue from your body
- Marking the area with ink (tattoo) so that it can be found again with future endoscopic exams
During the procedure
During an endoscopic mucosal resection, you can expect the following:
- Your role. You’ll be asked to change into a gown before the procedure. During the procedure, you’ll lie on your side on a cushioned table.
- Local anesthetic. If the endoscope is inserted through your throat, you may have your throat sprayed or be asked to gargle a solution to numb your throat to make insertion of the endoscope more comfortable.
- Sedation. You’ll be sedated during the procedure. With moderate sedation that causes you to be relaxed and drowsy, you may feel slight movement or pressure during the procedure, but you shouldn’t feel pain. Or you may be heavily sedated. Discuss with your gastroenterologist which option is appropriate for you.
- Monitoring. Nurses or other professionals will monitor your heart rate, blood pressure, blood oxygen level and comfort while the doctor performs the procedure.
After the procedure
You’ll remain in a recovery room until most of the effect of the sedative has worn off. You’ll receive written instructions about when you can start eating and drinking and when you can resume normal activities.
Relatively mild side effects may occur within 24 hours after the procedure including:
- Reactions to the sedative. You may continue to feel drowsiness and may experience nausea and vomiting.
- Sore throat. If the endoscope was guided down your esophagus, your throat may be sore.
- Gas or cramps. If air was pumped into your digestive system to make it more accessible, you may have gas, bloating or cramps after the procedure.
You’ll also receive written instructions about when to call your doctor or get emergency care after the procedure. The following signs or symptoms may indicate a serious complication from endoscopic mucosal resection:
- Fever
- Chills
- Vomiting
- Black stool
- Bright red blood in the stool
- Chest or abdominal pain
- Shortness of breath
- Fainting
Results
You’ll likely have a follow-up appointment with the gastroenterologist to discuss the outcome of your endoscopic mucosal resection and laboratory tests performed on lesion samples. Questions to ask your doctor include:
- Were you able to remove all abnormal tissues?
- What were the results of the laboratory tests? Were any of the tissues cancerous?
- Do I need to see a cancer specialist (oncologist)?
- If the tissues are cancerous, will I need additional treatments?
- How will you monitor my condition?
Follow-up exams
Typically, a follow-up exam is performed three to 12 months after your procedure to be sure the entire lesion was removed. Depending on the findings, your doctor will advise you about further examinations.
An exam will likely include a visual inspection with the use of an endoscope. Your doctor may mark the area of the removed lesion with ink (tattoo) so that when follow-up endoscopy is performed, he or she can be sure the lesion was removed completely.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
